Cardiovascular & Energy Systems: Heart & blood vessels
Blood vessels:
 Arteries Arteries
Arteries always carry blood away from the heart, either to the lungs, or to the
rest of the body. Arteries are responsible for delivering energy (nutrients) to
the whole body. All arteries carry oxygenated blood, except from the pulmonary
artery. Arteries have more smooth muscle, and thicker walls than other vessels
as well as containing a lot of elastin as they need to withstand high pressures
of blood being pumped out of the heart.
Arterioles
Arterioles connect arteries to the capillary network. Arterioles control the
flow of blood with the large amounts of smooth muscle in their walls by using
two processes known as vasodilation (dilation of the blood vessels) and
vasoconstriction (constriction of the blood vessels). Due to these processes,
arteries are able to control blood pressure and thermoregulation. They do this
by constricting or dilating in certain places, to move blood closer to the
surface of the body (when hot) or further from the surface (when cold).

Capillaries
Capillaries are the smallest vessels in the body with its walls at one
epithelial cell thick. Capillaries receive their blood from the arterioles and
feed to the Venules. Because of the thin capillary walls, the exchange of gases,
fluids and nutrients happens in the capillaries as they can diffuse through the
walls of the capillaries. Oxygen enters the capillaries from the arterioles and
leaves though the capillary walls, into muscles or organs, whilst CO2 enters the
capillaries through the capillary walls and leaves through the Venules.
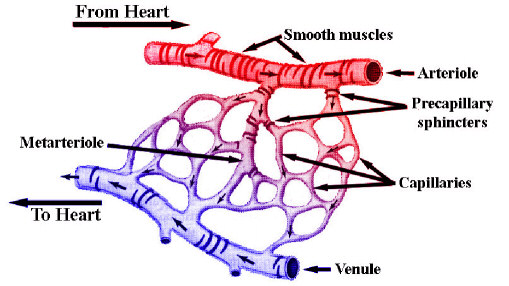
Venules
Venules allow outflow of blood from the capillaries, and have many connective
tissues in their walls, as the Venules move further away from the capillaries,
they become larger and connect with other Venules and eventually merge into
veins.
Veins
Veins have thinner walls, less smooth muscle and a thicker tunica externa than
arteries or arterioles as they do not need to withstand high pressures as the
blood in them can be forced back to the heart with the blood-muscle pump. Veins
have valves all along their inside, this is stop the back flow of any blood and
aid the blood-muscle pump and to help avoid blood pooling in the veins, as
depicted in the picture below:

Blood pressure:
|
Blood pressure is the measurement of force applies to
artery walls.

|
Blood pressure is measured as the pressure acting on the walls of the artery as
blood flows through it. Blood pressure results from two forces:
- The force of the blood as it is pumped out of the heart.
- And the other is the force created by the arteries to resist the blood flow.
During exercise, cardiac
output and blood pressure both increase, however, there are biological
mechanisms in place to prevent blood pressure from rising too high.
Vasoconstriction and vasodilation both act upon the blood vessels, altering the
blood pressure in different areas of the body to direct the majority of blood
flow to the muscles that require it.
|
There are 2 main methods of measuring blood
pressure, with auscultatoric and oscillometric instruments.
Below is using an Auscultatoric:

|
Blood pressure is measured with two
readings, these are systolic pressure (the pressure exerted when the heart
contracts) and diastolic pressure (the pressure exerted when the heart relaxes).
High blood pressure (Also called hypertension) is when blood pressure is
measured at above 140/90 mmHg (Systolic/diastolic). Prehypertension means you do
not have high blood pressure, but are likely to develop it in later life. A
blood pressure between 120/80 mmHg and 139/89 mmHg is considered to be
Prehypertension. Blood pressure can also be affected by the ANS (autonomic
nervous system), more specifically the SNS (sympathetic nervous system) as this
can be triggered by the stress of having your blood pressure measured and can
cause an increase in blood pressure.
Structures in the Heart
There are two atria in the heart, the left atrium, and the right atrium. These
are both small chambers at the top of the heart that hold blood until the atrio-ventricular
valves open, letting blood through to the ventricles. The atria receive blood
through veins, the vena cava on the right, and the pulmonary vein on the left.
There are two atrio-ventricular valves. These are the Bicuspid valve, and the
Tricuspid valve. The bicuspid valve is in the left side of the heart, and
separates the left atrium from the left ventricle. The bicuspid valve is made up
of two flaps, whilst the Tricuspid valve is made up of three flaps. The
tricuspid valve is the other atrioventricular valve, and separates the right
atrium from the right ventricle. Both of these valves hold blood in the
atria until the valves open due to atrial systole (contraction of the atria),
forcing blood into the ventricles. Then valves then act to prevent blood flowing
back from the ventricles into the atria during ventricular systole (contraction
of the ventricles).

There are two ventricles in the heart, again, one on the left, and one on the
right. The left ventricle needs to pump harder than the right ventricle as blood
from the left ventricle needs to travel around the entire body, whilst blood
from the right ventricle only needs to be pumped as far as the lungs. Both
ventricles receive the blood that they pump, from the atria directly above them.
The septum is a thick muscular tissue separating both sides of the heart; the
septum stretches from the bottom right to the top of the heart, changing from
the interventricular septum (separating the ventricles) to the interatrial septum
(separating the atria).
There are two semi lunar valves; these are called the aortic semi lunar
valve, and the pulmonary semi lunar valve. The aortic semi lunar valve separates
the left ventricle from the aorta, and much like the atrioventricular valves,
they stop blood flowing back from the aorta into the left ventricle. The
pulmonary semi lunar valve separates the right ventricle from the pulmonary
artery and again, stops the back flow of blood, this time between the arteries
to the ventricles.
|
X-ray of heart:

|
How the heart beats:
The heart is made up of a certain muscle type called cardiac muscle. This
specific type of muscle has one major advantage. Due to the very high amount of
mitochondria found, cardiac muscle never tires. The large amount of
mitochondria is also why cardiac muscle appears to have a reddish colour.
The heart is naturally myogenic. This means that it does not require a
stimulus from outside itself and can contract and relax without nervous
stimulation. This is because of the Sino-Atrial Node.
The Sino Atrial Node (SAN) is the natural pacemaker for the heart. The SAN is
located in the upper area of the right atrium, and creates an electrical impulse
to start the beat of the heart. This impulse then travels through the walls of
the atria, causing atrial systole (contraction in the walls of the atria) which
forces the blood through the atrio-ventricular valves, and into the ventricles.
Once the electrical impulse has passed through the walls of the atria, the
atrial walls can begin to relax (atrial diastole) and the atria can begin to
fill with blood again. This impulse then reaches the Atrio-Ventricular Node (AVN)
and is redirected down the Bundle of His, towards the purkynje fibres. Once it
reaches the purkynje fibres, the impulse is then conducted along the purkynje
fibres, around the walls of the ventricles, starting from the bottom and moving
upwards, causing ventricular systole (contraction of the ventricles) forcing
blood upwards and into the arteries, either the Pulmonary Artery or the Aorta.
Once the electrical impulse has passed through the ventricles, it stops and the
ventricles begin to relax (ventricular diastole), the ventricles are then ready
to receive the blood that has stored up in the atria, when the next impulse is
sent out by the SAN. This process is repeated each time the heart beats.
Cardiac functions
Thermoregulation:
 Thermoregulation is the control of temperature in the body and is achieved
through the process of vasodilation and vasoconstriction. When the body becomes
cold, it prioritises the important organs and areas of the body, and so
vasoconstriction occurs in vessels closer to the surface of the skin, especially
in areas like the fingers, or tip of your nose. When the vessels in these areas
constrict, the blood flow directs more towards the core of the body, so the hot
blood helps to maintain the core temperature of the body, which could be
lifesaving. Thermoregulation is the control of temperature in the body and is achieved
through the process of vasodilation and vasoconstriction. When the body becomes
cold, it prioritises the important organs and areas of the body, and so
vasoconstriction occurs in vessels closer to the surface of the skin, especially
in areas like the fingers, or tip of your nose. When the vessels in these areas
constrict, the blood flow directs more towards the core of the body, so the hot
blood helps to maintain the core temperature of the body, which could be
lifesaving.
When the body is hot, vasodilation occurs in the vessels closer to the
surface of the skin, this allows the blood in these vessels to cool down, as the
blood is closer to the cooler external environment. The cooler blood then
continues around the body, cooling it down.
Arterioles are the main vessel involved with thermoregulation, this is
because they have the highest percentage of smooth muscle of all the blood
vessels and so can dilate or constrict more than other vessels can.
Transportation of blood and removal of metabolic waste:
 This function involves the removal of CO2, heat and H2O to the lungs and
kidneys. Blood delivers oxygen, heat, hormones, nutrients and minerals and to
areas of the body that require it, as well as maintaining body temperature and
balance (homeostasis). During exercise, there is an increase in the muscle's
demand for blood containing oxygen and different nutrients and minerals, there
is also an increased demand for removal of CO2 from the body, as it is toxic to
the body. The body reacts to this, by increasing the blood supply to this area
of the body, which subsequently increase the levels of oxygen, nutrient and
minerals as well as the increased amounts of CO2 being removed from the body. This function involves the removal of CO2, heat and H2O to the lungs and
kidneys. Blood delivers oxygen, heat, hormones, nutrients and minerals and to
areas of the body that require it, as well as maintaining body temperature and
balance (homeostasis). During exercise, there is an increase in the muscle's
demand for blood containing oxygen and different nutrients and minerals, there
is also an increased demand for removal of CO2 from the body, as it is toxic to
the body. The body reacts to this, by increasing the blood supply to this area
of the body, which subsequently increase the levels of oxygen, nutrient and
minerals as well as the increased amounts of CO2 being removed from the body.
Increased heart rate during exercise:
The heart rate is the amount of beats per minute an individualís heart makes. At
rest, a normal adultís heart beats around 75 beats per minute, and this can
increase to around 200 beats per minute during strenuous exercise. This increase
during exercise is due to the higher demand for oxygen in the muscles, and to
help remove increased levels of CO2 from the body at a faster rate.
The heart rate is controlled by the SAN (Sino atrial node). The heart rate
changes when the SAN receives signals from the medulla, via the sympathetic or
parasympathetic nervous systems.

The sympathetic nerve speeds up the heart rate
by releasing a hormone called noradrenalin from the synapses at the end of the
nerve, stimulating the heart to beat at a faster rate. When the sympathetic
nervous system is active, most core bodily functions are slowed, e.g. digestion
is slowed, which allows more of the bodyís blood to be redirected to the areas
that require it. The Vagus nerve (parasympathetic nerve) slows the heart rate
back to its resting rate by releasing a hormone called acetylcholine. When the
parasympathetic nervous system is active, breathing rate is slowed and digestion
returns to its resting rate. The sympathetic and parasympathetic nervous systems
are both activated by the medulla in the brain.
Chemoreceptors in the carotid and aortic bodies detect changes in the PH
level of blood. An increase in CO2 in the blood will increase the bloods acidity
(decrease the PH) and this change will be picked up by the chemoreceptors. These
receptors then send a signal to the medulla, causing the medulla to either
activate the sympathetic nervous system, or the parasympathetic nervous system.
Other receptors within the body that can also affect heart rate are
mechanoreceptors. These receptors can be found in the joints and ligaments of an
individual, and send feedback of the movement occurring at each joint, to the
medulla, which can then cause an increase or decrease in heart rate via the
sympathetic or parasympathetic nervous systems.
There are two main nervous systems in the body; these are the autonomic
nervous system (ANS) and the voluntary nervous system (sometimes known as the
somatic nervous system).

The autonomic nervous system is split up into two
sections; the first of these is the sympathetic nervous system (SNS). The SNS
increases heart rate and breathing rate. The SNS is activated by emotional or
physical stress on the body, this causes a release of Noradrenalin (NAd) which
increases the work rate of the heart. Due to this increase of heart and
breathing rates, the body slows down digestion to allow more blood and oxygen to
get to the heart and lungs. The second part of the nervous system is the
parasympathetic nervous system (PNS), this system reduces heart, and breathing
rates. It also resumes normal digestion patterns and is also responsible for
returning the body to a balanced state (homeostasis). The PNS is activated when
the body needs to return to its resting state, after the SNS has been active for
a period of time. PNS responses are controlled by Acetylcholine, which acts as a
neurotransmitter in the PNS, causing an increase or decrease in the levels of
activity in the PNS.
Increase in Stroke volume during exercise:
Stroke volume is the volume of blood pumped out of the left ventricle in one
cardiac cycle. Around two thirds of the blood in one ventricle is pumped out
with each beat, this volume progressively increases during exercise until it
plateaus at a higher level, and will gradually return to normal after the
exercise is finished. This increase in stroke volume allows the body to remove
CO2 from the muscles faster, as well as delivering higher amounts of oxygen to
the muscles that require it. The stronger an individualís heart is, the larger
volume of blood is pumped out of the heart with each beat. So a trained athlete
will most likely have a higher stroke volume than an untrained athlete.
Increase in Cardiac output during exercise
 Cardiac output is the amount of blood pumped from the heart in one minute. It is
equal to stroke volume multiplied by heart rate (If a heart beats 65 times in
one minute, and has a stroke volume of 80ml per beat, then the cardiac output
would equal 65 X 80 = 5200ml per minute. The average adultís resting cardiac
output is 4900ml per minute; however, cardiac output may reach up to 30 litres
per minutes during extreme exercise. Increased sympathetic nervous system
activity and decreased parasympathetic nervous system activity, resulting in an
increased heart rate, would increase the cardiac output. Cardiac output is the amount of blood pumped from the heart in one minute. It is
equal to stroke volume multiplied by heart rate (If a heart beats 65 times in
one minute, and has a stroke volume of 80ml per beat, then the cardiac output
would equal 65 X 80 = 5200ml per minute. The average adultís resting cardiac
output is 4900ml per minute; however, cardiac output may reach up to 30 litres
per minutes during extreme exercise. Increased sympathetic nervous system
activity and decreased parasympathetic nervous system activity, resulting in an
increased heart rate, would increase the cardiac output.
|
Red Blood Cells:

|
Blood composition:
Blood makes up about 8% of our body weight, ranging from 4-6 liters of blood
(4-5 for females, 5-6 for males). Our blood is regulated through the process of
homeostasis, to keep the blood at a temperature of 38 degrees. Blood is around 5
times more viscous than water and contains plasma, erythrocytes, hemoglobin,
leucocytes and thrombocytes.
Plasma makes up 55% of the blood volume and is a mixture of proteins,
enzymes, nutrients, waste toxins, hormones and gases, but is composed mostly of
water (93%), and is a straw color in appearance. Plasma contains three main
proteins; these are albumins, globulins and fibrinogen.
Erythrocytes, also known as red blood cells, take and release oxygen into the
capillary beds, as well as carrying Co2 back to the lungs to be removed from the
body.
Hemoglobin is an oxygen transport protein that gives blood its red
color.
Oxygen attaches onto the hemoglobin which is attached to the erythrocytes.
Hemoglobin carries oxygen from the lungs to the rest of the body, and carries
CO2 back to the lungs. One erythrocyte contains about 250,000,000 hemoglobin.
|
Leucocytes and Red Blood Cells:

|
The primary function of Leucocytes, also known as white blood cells, is to
fight off diseases that enter the body, but they can also inhibit the growth of
bacteria and help to prevent blood clotting. Leucocytes make up 1% of the volume
of blood, but can be easily multiplied to fight infection.
Thrombocytes (platelets) are the main part of the blood clotting process, and
are initiated following a trauma. The thrombocytes trap erythrocytes in the
clot, to form a scab, protecting the wound and allowing time for the body to
heal. The protein Thrombonin is a factor that helps form a blood clot.
Energy systems
As exercise varies in intensity, different energy systems need to be used. There
are three different energy systems within the body; these are the aerobic energy
system, the lactic acid energy system and the phosphor-creatine energy system.
Aerobic energy system:
 The aerobic energy system is active when the heart is working at 50% of its
maximum output or below, and can keep working at this intensity for very long
periods of time. The aerobic energy system requires oxygen to breakdown the
glucose or fat. The energy is produced within the mitochondria inside the cells
in the body. When one oxygen molecule aids the breakdown of 1 glucose molecule,
38 molecules of ATP are produced, but when one oxygen molecule is used to
breakdown one fat molecule, 129 molecules of ATP are produced. The high amount
of ATP being produced each day (120,000,000,000,000,000,000,000,000) is the
reason behind the aerobic energy system being able to work for very long periods
of time. If this energy system is used to its limits then the recovery time is
the longest of all energy systems and can sometimes take up to three or four
days. The aerobic energy system is active when the heart is working at 50% of its
maximum output or below, and can keep working at this intensity for very long
periods of time. The aerobic energy system requires oxygen to breakdown the
glucose or fat. The energy is produced within the mitochondria inside the cells
in the body. When one oxygen molecule aids the breakdown of 1 glucose molecule,
38 molecules of ATP are produced, but when one oxygen molecule is used to
breakdown one fat molecule, 129 molecules of ATP are produced. The high amount
of ATP being produced each day (120,000,000,000,000,000,000,000,000) is the
reason behind the aerobic energy system being able to work for very long periods
of time. If this energy system is used to its limits then the recovery time is
the longest of all energy systems and can sometimes take up to three or four
days.
Lactic acid energy system:
Glycolysis is the breakdown of glucose stored in the muscles and liver (known as
glycogen). The energy produced from this breakdown is used as energy for
the muscles. When glucose is broken down, it produces 2ATP molecules, and when
glycogen is broken down, it produces 3 ATP molecules. The lactic acid system
lasts 60-90 seconds during high intensity exercise, and has a recovery time of
around 1 hour, but this recovery time can be reduced with an appropriate cool
down. Pyruvic acid is the by-product of this reaction, which is used in the kreb
cycle.
Phospho-creatine energy system:
Phosphocreatine is made up of one phosphate and one creatine molecule. When the
phosphocreatine energy system is used the phosphate from the phosphocreatine is
donated to an ADP (Adenosine Diphosphate) molecule, causing it to instantly re-synthesise
into an ATP (Adenosine Triphosphate) molecule, ready to be broken down again.
Stored within the muscles there is enough phosphocreatine to last five to ten
seconds of maximum output and so this energy system is only used for very short,
high intensity (maximum) output. The phosphocreatine within the muscles is
restored quickly after it has been used.
Thanks for reading, and I hope you are now a little bit more educated on the
cardiovascular system and how the heart functions!
Biology
An Introduction to the Cells of Organisms
Cardiovascular System and Energy Systems |